December 8th, 2021
One thing we’ve learned about COVID-19 is that children experience the infection differently than adults. Because of reasons still not fully understood, infections in kids are more likely to cause little or no symptoms, whereas adults are more likely to have complicated clinical courses resulting in poor outcomes. Complications and deaths in the pediatric population are thankfully very rare, although COVID-related MIS-C (multisystem inflammatory syndrome in children) remains a concern on the minds of pediatricians and parents, and stubborn symptoms can persist for months in pediatric long-haulers. Regardless, the American Academy of Pediatrics emphasizes that “all children and adolescents who test positive for SARS-CoV-2 should notify their pediatrician.”
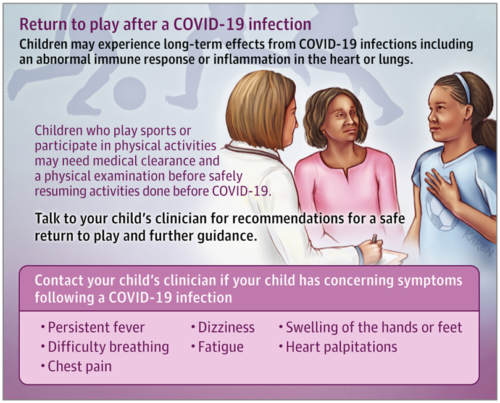
Even though their symptoms might seem trivial, it is still important to treat children carefully as they recover from COVID-19. In particular, student athletes who test positive for the virus should be subject to fairly strict protocols before they are allowed to return to sports.
Over the summer, the American Academy of Pediatrics Council on Sports Medicine and Fitness updated its guidance on returning students to youth sports after COVID-19 infections. Ryan Basen says the AAP hopes to “maximize the health of everyone involved (athletes, coaches, parents, other fans, and referees), while allowing kids to play.”
The group is asking participants to wear masks whenever possible and to get vaccinated if they are 12 and older. “Outdoors, people should be spacing out; we still don’t want people sharing water bottles,” Briskin noted. Spectators should also don masks, even outdoors. In addition, they are recommending that “decisions be made on a local level when considering cancellations, delays, or limitations,” according to the guidance.
For children who test positive for SARS-CoV-2, the AAP advises the following medical evaluations before clearing kids to participate in organized sports and physical fitness classes in school:
For a child or adolescent who is SARS-CoV-2–positive who is either asymptomatic or mildly symptomatic (<4 days of fever >100.4°F, <1 week of myalgia, chills, and lethargy) a phone or telemedicine visit with the pediatrician is recommended, at a minimum, so appropriate guidance can be given to the family.
For those with moderate symptoms of COVID-19 (≥4 days of fever >100.4°F, ≥1 week of myalgia, chills, or lethargy, or a non-ICU hospital stay and no evidence of multisystem inflammatory syndrome in children [MIS-C]), an evaluation by their primary care physician (PCP) is recommended. People who test positive for SARS-CoV-2 should not exercise until they are cleared by a physician.
For children and adolescents with severe COVID-19 symptoms (ICU stay and/or intubation) or MIS-C, it is recommended they be restricted from exercise for a minimum of 3 to 6 months and obtain cardiology clearance prior to resuming training or competition.
Regardless of the severity of their kid’s bout with COVID-19, parents should be on the lookout for problems when the child starts exercising again:
All children and adolescents and their parents/caregivers should be educated to monitor for chest pain, shortness of breath out of proportion for upper respiratory tract infection, new-onset palpitations, or syncope when returning to exercise. If any of these signs and/or symptoms occur, the AAP recommends immediately stopping exercise and the athlete should see their pediatrician for an in-person assessment. Consideration should be given for pediatric cardiology consultation.
The AAP recommends a gradual, stepwise progression to return to play:
Stage 1: Day 1 and Day 2 – (2 Days Minimum) – 15 minutes or less: Light activity (walking, jogging, stationary bike), intensity no greater than 70% of maximum heart rate. NO resistance training.
Stage 2: Day 3 – (1 Day Minimum) – 30 minutes or less: Add simple movement activities (eg. running drills) – intensity no greater than 80% of maximum heart rate.
Stage 3: Day 4 – (1 Day Minimum) – 45 minutes or less: Progress to more complex training – intensity no greater than 80% maximum heart rate. May add light resistance training.
Stage 4: Day 5 and Day 6 – 2 Days Minimum) – 60 minutes: Normal training activity – intensity no greater than 80% maximum heart rate.
Stage 5: Day 7 – Return to full activity/participation (ie, contests/competitions).
Read “Youth Sports: A COVID-19 Safety Checklist” from the AAP here.
(Image: JAMA Pediatrics Patient Page)