Please could you introduce yourself and tell us what inspired your latest research into COVID-19?
My name is Paolo De Coppi. I am a pediatric surgeon, working mainly with children that have congenital or sometimes acquired diseases, treating them with surgery when possible.
At the beginning of the pandemic, while it was quite clear that COVID did not mainly affect children, we had a number of children presenting with symptoms that were similar to appendicitis, but without its classical features.
We started imaging this and discovered that there was a slightly different manifestation of COVID in children that was more focused on the GI tract. There were big lymph nodes in these children’s tummies, and that was what was causing tummy pain, not appendicitis. We reported our observations in a letter to the Lancet early in the pandemic in the Lancet Child and Adolescent Health issue.
I wanted to know why children did not have respiratory symptoms in this manifestation, only GI symptoms. Soon after that, a few publications were showing that SARS‑CoV‑2 could actually replicate in the GI tract. For me, it was important to understand how the virus circulated from the airway to the stomach, to the intestine. The point of entry to the intestine is the stomach. We wanted to determine whether the virus could replicate there because, in that way, children also can be passing on the disease oral-fecally, rather than through classical respiratory transmission.
We are a tissue engineering laboratory. We work with cells to build tissues and organs enabling us to test hypotheses with various organs, particularly on the GI tract. At that time, we had just had a paper accepted on building an intestinal mucosa with Vivian Lee in Nature medicine. We thought that if we could build a sort of mini stomach, we could test this hypothesis.
Next, we collaborated with one of the groups in Italy that first isolated the COVID virus in the first wave of the pandemic. We sent over this engineered mini gut model and they were able to not only infect them but also show that the virus was happily replicating, particularly in organoids derived from children.
Image Credit: visivastudio/Shutterstock.com
COVID-19 has had a huge impact on many sectors within science with many researchers adapting their focus to help understand the virus in more detail. Why did you want to help contribute to the global fight against COVID-19?
I think all doctors and people in the field of biomedicine, from nurses to scientists, felt their responsibility to help in this unique situation. We all wanted to use our skills to help where we could. At that time I had a lot of people in the lab from all over the world who felt useless to just be at home, not being helpful, because classical research could not continue. We wanted to help.
We thought that these engineered tissues we had in the laboratory could be used to test infection, in collaboration with experts on the virus, to try to understand what was going on better. It was very rewarding for everyone in the lab to see that what they were making was useful both from an engineering perspective and as a tool for understanding the infection. This was extremely rewarding from a personal point of view because it felt like we were doing something significant.
Can you describe what is meant by the term organoids and where they are typically used within health and science?
Organoids are like small organs, although they cannot replicate all the functions of the organs. You can culture cells from a tissue or an organ in a spheroid. These spheroids form to replicate some of the functions of the organs, and typically, these are the most important functions.
For example, for the gut, one of the most important functions is that of the epithelium because the epithelium absorbs the nutrients and carries out digestion. The organoids need to include the epithelium of the gut. The gut grows as small organs in which most of the functions of the epithelium are replicated.
That is what happened with the virus. The virus penetrates through the epithelium of the intestine. Therefore, if you can replicate that in vitro, you can show how the infection works.
How invaluable are these organoids to research? What advantages do they have when studying organ function?
Organoid research has taken over, thanks to some of the leading laboratories in the world. One of those that I want to mention because it was one of the first studies on the epithelium of the gut is Hans Clevers in Utrecht. He is one of the leaders in this field who showed that you can take a biopsy from an intestine and then grow these organoids, almost forever in culture.
This is extremely useful because you can understand not only the normal physiology of the gut but you can, for example, study why a cancer developed from a particular epithelium. You can study what happens when dysregulation comes into place.
You can also study diseases like we have done, for example, infection. Inflammatory bowel disease can also be studied, or you can study situations where you have an ischemic event and you have damage to the epithelium or the intestine. Therefore you can see how the epithelium regenerates and replicates.
The role of the gastrointestinal system in biological processes, such as healthy brain function, has received interest recently. Could you discuss why it is important to model how this organ functions and how important it is to our overall health?
We are touching on something here that has not been explored completely yet. There is a so called gut brain access, and this is regulated in some way. The studies out there seem to show that, for example, the bacteria growing in your gut can condition some of the brain function.
This is something that needs to be explored further as at the moment things are not so clear. This organoid model may help with the understanding of how some of the secretory factors of the epithelium in the gut may condition other cell types, like the organoids of the brain. This is really at the cutting edge of research. Some groups are working on this, but there is not yet a clear representation of how the gut influences the brain through this access.
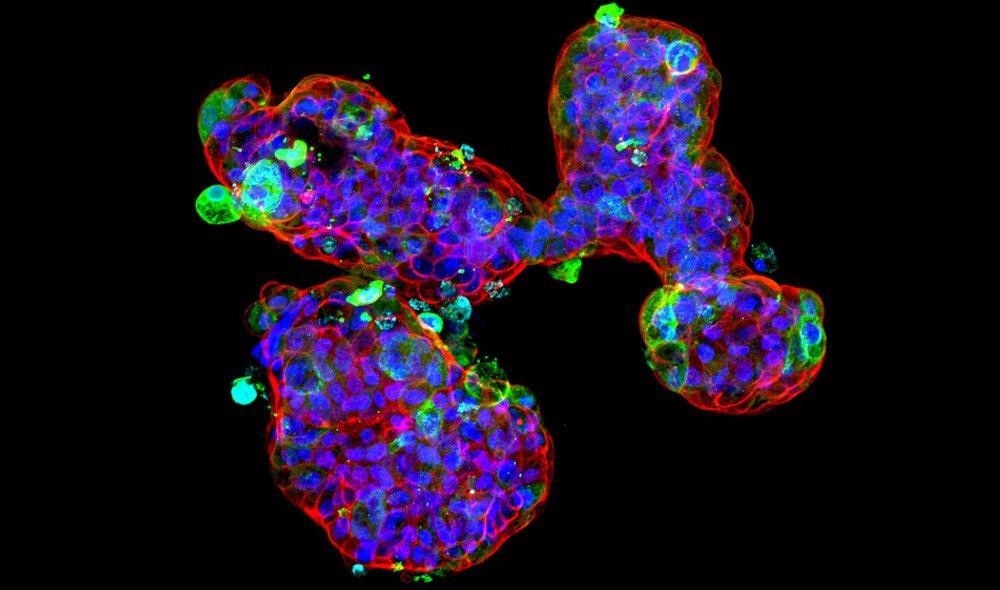
Image Credit: Giovanni Giobbe
In your latest research, you grew a mini stomach organoid across different stages of human development. Can you describe how you grew these mini stomachs and how you were able to represent the varying stages of human development?
This is very important and is thanks to the access to the material here that we have in the UK. I think it is pretty unique that we have access to the developing stages of a human fetus. This is so important because it helps us to understand how the human gut develops. While there are similarities with other mammals, the human gut has some important unique differentiation pathways from other species.
We were able to obtain tissues from the early phase of development and early in the postnatal period from tissue that was discarded from surgery, as well as adult tissue from biopsies. Then we were able to form organoids from all these stages of development, discovering that the behavior of these organoids was understandably very different at different stages. The pediatric cells actually have some similarities with the fetal cells, which are completely lost in the adult.
Viral replication was observed to be more noticeable in cells growing from child and late fetal cells compared to adult and early fetal cells. Why might this be?
This is an important question. We have demonstrated the differences, but what we do not know yet is the reason for those differences. It looks like the naïve stem cells in the fetus and pediatrics express receptors that are useful to the virus for getting in. In the adult, the cells lose this expression.
Once we grow the cells and make them different from a specialized epithelium, a specialized mucosa, these differences disappear. As progenitors, there are receptors that the virus needs to enter into the cells that are not there in the adult, so that is something that is clearly different. Why is this different? We do not know yet.
The growth of organoids, particularly those that can replicate a fully-functioning organ, can sometimes be a difficult process. Did you encounter any challenges during your investigations and how were they overcome?
One very clear answer to this is the polarization of the organoids. When you grow organoids, they grow like a sphere. This sphere has the epithelium that is normally present in the intestine looking inside. The lumen inside the sphere is the lumen of the tube of our intestine or our gut in general.
The problem with this is that when we started infection in this way, we could not see much infection because the surface of the epithelium was inside the sphere. The virus could not gain access easily. We had to invert the polarization of the epithelium and make the organoids look inside out.
When we changed that we saw much more efficient SARS-CoV-2 infection in the organoids. This was a clear biological answer to the question: how can we improve the infection rate and make it similar to in vivo?
How was your mini stomach organoid used to study the gastrointestinal impacts of SARS-CoV-2? What did you discover when studying this?
We believe the next step will be to have these organoids for two things. The first is as a predictive model. We are seeing just now with the Omicron strain the different mutations the virus can have. It can lead to completely different clinical manifestations. Can we predict the way that the virus behaves with these in vitro models? We are really keen to study the different variants with this model and see if they have a different impact on different ages or systems.
The second thing is can we use some protectors, for example, to decrease the virus penetration to the epithelium. This is outside my field of expertise, but we can offer this model to a specialized lab that can work on this. We want to get more funding to try to use this system for predictions within this and other pandemics.
Image Credit: Corona Borealis Studio/Shutterstock.com
Do you believe that your research will help to further our understanding of the impacts COVID-19 has on the gastrointestinal system?
I strongly believe that this is very important for that. At the moment, for example, we are observing a lot of young people and children getting infected and some of them may have negative swabs in their airway because that is not the primary target of the virus.
I think our model can further help understand this problem and the role of the GI system in the pandemic, particularly in children.
Could your lab-grown mini stomachs also be used to continue studying the stomach and how it develops over time? Are there any applications where this would be particularly beneficial?
We are trying to go back to the primary aim of this work, which is to engineer mini stomachs. Mini stomachs will be beneficial for children that are born without a stomach or have a very small stomach. In the operation where we make the stomach bigger, we use the intestine, but the intestine is a different part of the body and does not work in the same way as the stomach. Those children continue to have problems.
Adults can also lose their stomachs, for example, because of cancer. At the moment, to treat this the stomach is completely taken out and replaced with the intestine, but those adults struggle to feed because they do not have a sac to digest the food. By doing this research, we could reach a stage where we could replicate the stomach.
In the meantime, developing a more complex stomach, for example, including inflammatory cells or endothelial cells, could help us understand the relationship between COVID-19 and other cell types that are present in the stomach more. We know that, for example, the endothelium can be affected. We know that there has been a local reaction described. We want to see if those types of manifestations can be replicated in vitro.
What are the next steps for you and your research?
The first direction is to acquire more funding and to use these organoids as a model to test the different variants, in particular how the different variants work in a child’s stomach. That could help predict what will happen in the future and understand if this is a minor disease to the GI tract, or if it can actually lead to cell death or cell apoptosis, and so on.
The second direction is within regenerative and tissue engineering in which we are trying to create a more complex mini stomach that could be used to replace missing stomachs in both adults and children.
Is there anything else at all you wanted to add?
This is a work of many and it is all thanks to collaborating with people of different expertise. To get through difficult moments, the best thing to do is to create networks, as many have done, and try to answer questions by working together.
If you want to find a positive element from this pandemic, there has never been a better moment in science than this, as it has really pushed people to work together.
About Paolo De Coppi
Paolo De Coppi is the Nuffield Chair of Paediatric Surgery, the NIHR Professor of Paediatric Surgery, and Consultant Paediatric Surgeon at the Great Ormond Street Hospital. He is the President Elect of the European Pediatric Surgical Association and the Head of the Surgery Unit, Stem Cells & Regenerative Medicine Section, Developmental Biology& Cancer Programme at the UCL Great Ormond Institute of Child Health. In 2020 he has become the first Paediatric Surgeon to be elected Fellow of the Academy of Medical Sciences.
Professor De Coppi trained at Boston Children’s Hospital, the Academic Medical Center (Amsterdam, NL), and Padua University (Italy), and has a special interest in congenital malformations and their treatment using minimally invasive techniques. He is a patron for TOFS and CDHUK and has focused his research interests on stem cells and tissue engineering by trying to find new modalities for the treatment of complex congenital anomalies.
He identified stem cells from amniotic fluid and he has described methods to decellularised several organs and tissue such as the kidney, intestine, liver, pancreas, and lung. In 2010 he was part of the team that performed the first successful transplantation of a tissue-engineered trachea on a child at the Great Ormond Street Hospital. He has published more than 350 peer-reviewed articles (h-index 65) in journals such as Nature, Nature Biotechnology, The Lancet, Nature Biomedical Engineering, Nature Communications, and Cells Stem Cells; supervised more than 35 research fellow and Ph.D. students; and has been awarded various national and international grants in excess of £30 million. He is on the editorial boards of Stem Cell Development, Journal of Pediatric Surgery, Pediatric Surgery International, and Fetal and Maternal Medicine Review. As of 2011, he has been the senior associate editor for Stem Cell Translational Medicine.




-1.jpg)