December 13th, 2021
As we come up on the second anniversary of COVID-19 — on December 31, 2019, the World Health Organization reported a cluster of cases of pneumonia caused by a novel coronavirus subsequently identified as SARS-CoV-2 — it’s now clear that humans will be battling the virus for many years to come. Part of the reason is that the virus is constantly changing, mutating to form new versions of itself faster than scientists and public health authorities can react.
Another explanation for COVID-19’s staying power is that the vaccine — available everywhere in the United States at no cost to its citizens — has barely penetrated populations in developing countries. Ultimately, we know that coronavirus won’t be defeated here until it is defeated everywhere.
Even with widely available vaccines, many people are still reluctant to get it for a variety of reasons: political ideology, religious beliefs, distrust of science and institutions, inconvenience, and other personal excuses that often rely on misinformation or intentional disinformation. Although the number of people not getting a jab due to a medical contraindication is low– the only true “red light,” anaphylaxis to the vaccines’ ingredients, is exceedingly rare — there are individuals who believe, despite evidence to the contrary, that receiving a COVID vaccine could potentially put them at risk for an adverse side effect or an exacerbation of their medical condition.
Doctors who treat patients with chronic health conditions play a huge role in coaxing their worried patients to get vaccinated, even if the process takes some time. However, pregnancy is one pre-existing condition where there is little time to waste to prevent this dangerous respiratory virus.
It’s easy to understand why women who are pregnant might balk at taking a new vaccine designed to defend against a brand new virus. After all, for anyone wishing to introduce new medications or substances into their bodies, pregnancy certainly isn’t the time. Gavi points out that COVID-19 presents a challenge to young parents who just want to do the right thing and have a good birth outcome:
Avoiding non-essential medicines may not have major consequences most of the time, but this is not the case for the COVID-19 vaccine. The World Health Organization advises pregnant women to take the vaccine as the disease can increase the risk of babies being born prematurely or having complications. Having COVID-19 while pregnant means being 20 times more likely to need intensive care, and one in five people put on a lung-bypass machine in England were unvaccinated pregnant women.
Kristen Walter, M.D, singles out pregnancy as a high-risk situation in light of COVID-19.
Pregnant and recently pregnant individuals with COVID-19 are more likely than nonpregnant people of similar age to require intensive care unit admission, mechanical ventilation, or extracorporeal membrane oxygenation (ECMO) through a machine that acts as an artificial lung. Pregnant people also have higher rates of death due to COVID-19. Risk factors for more severe illness and death among pregnant people with COVID-19 include older age, high body mass index, and preexisting comorbidities (such as high blood pressure and diabetes).
Infection with SARS-CoV-2 during pregnancy greatly increases the risk to the fetus by inducing preterm labor and delivery. Higher rates of fetal death have been documented; in the first 18 months of the pandemic, the CDC estimated the rate of stillbirths in American women with COVID-19 was double the rate compared with women without the infection during pregnancy.
The case for COVID-19 vaccine during pregnancy and lactation is now clear, even if the vaccines weren’t initially studied for those two situations. Enough is known now to reassure pregnant women about the safety of the vaccines:
None of the COVID-19 vaccines contains live virus, so pregnant people and fetuses cannot develop COVID-19 from vaccination. Moreover, ongoing monitoring of COVID-19 vaccination during pregnancy has shown no increase in miscarriage or other safety concerns in pregnancy and no adverse effects on fetal or postnatal development.
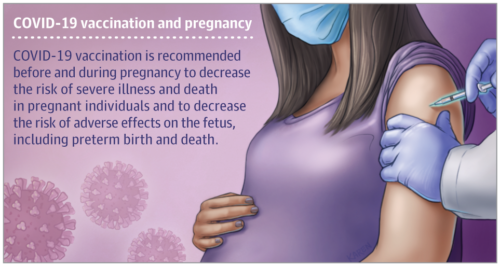
COVID-19 vaccination is recommended before pregnancy and any time during pregnancy to decrease the risk of severe illness and death in pregnant individuals and to decrease the risk of adverse effects on the fetus, including preterm birth and death.
With under 40% of pregnant women in the U.S. fully vaccinated, pediatricians, obstetricians, and maternal-fetal specialists feel a sense of urgency to get shots into the arms of women who are pregnant or trying to get pregnant now or in the future:
• The American College of Obstetricians and Gynecologists (ACOG) recommends that all eligible persons greater than age 12 years, including pregnant and lactating individuals, receive a COVID-19 vaccine or vaccine series.
• For patients who do not receive the vaccine, the discussion should be documented in the patient’s medical record. During subsequent office visits, obstetrician–gynecologists should address ongoing questions and concerns and offer vaccination again.
New moms who want to breastfeed are urged to get vaccinated and boosted, for their benefit as well as their baby’s:
COVID-19 vaccination is recommended for individuals who are breastfeeding to decrease their risk of COVID-19. In addition, people who receive an mRNA COVID-19 vaccine (Pfizer-BioNTech or Moderna) have been found to have antibodies in their breast milk, which may help protect infants from infection.
Like advanced age, obesity, diabetes, and hypertension, pregnancy is another risk factor that can make an already difficult-to-manage infection much worse. Women who are pregnant should talk it over with their obstetrician for reassurance that vaccination is the best path to a safe pregnancy and healthy outcome.
More PediaBlog on COVID-19 and pregnancy here.
(JAMA Patient Page — 12/10/21)