June 14th, 2022
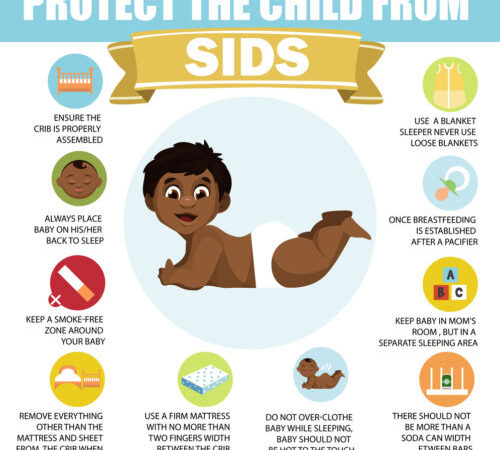
Roughly 3,400 infants under 1 year of age die suddenly and unexpectedly — mostly while they sleep — in the United States each year. According to the Centers for Disease Control and Prevention, these sudden unexpected infant deaths (SUID) are understood to be due to three factors:
1. Sudden infant death syndrome (SIDS)
2. Accidental suffocation in a sleep environment
3. Unknown causes
The PediaBlog highlighted effective prevention tactics back in 2015:
In 1992, researchers recognized that sudden infant death syndrome (SIDS) could be prevented simply by positioning babies to sleep on their backs rather than their sides or stomachs. Since then, the AAP’s “Back to Sleep” campaign has resulted in a dramatic decrease in SIDS deaths. Eliminating soft bedding and ensuring a safe sleep environment drives that number down further, but not completely. Clearly, there are other factors involved for other SIDS victims, and researchers are narrowing them down.
While SIDS deaths have declined significantly since the “Back to Sleep” program was adopted by pediatricians and parents in the U.S. and around the world, babies whose parents took every precaution to prevent a sudden unexpected death still die from SIDS.
Pediatric researchers in Australia looking at infants’ brain function may have found an important key to to help solve this tragic mystery. By testing blood sample from babies who died of SIDS, Rosemary Scott reports that the researchers may have found a revealing biomarker:
Each SIDS sample was then compared with blood taken from healthy babies. They found the activity of the enzyme butyrylcholinesterase (BChE) was significantly lower in babies who died of SIDS compared to living infants and other non-SIDS infant deaths. BChE plays a major role in the brain’s arousal pathway, explaining why SIDS typically occurs during sleep.
The study’s principle investigator had reassuring words for parents grieving an unthinkable loss:
“These families can now live with the knowledge that this was not their fault,” [Carmel Harrington, PhD] said.
In the study, the researchers wrote, “This finding represents the possibility for the identification of infants at risk for SIDS infants prior to death and opens new avenues for future research into specific interventions.”
Now that this biomarker has been further confirmed, researchers can turn their attention to a solution. In the next few years, those in the medical community who have studied SIDS will likely work on a screening test to identify babies who are at risk for SIDS and hopefully prevent it altogether.
While more research into this “breakthrough” finding is needed, Dr. Harrington is hopeful:
In a radio interview, Harrington said, “I know that in 3 to 5 years’ time, SIDS will be a thing of the past,” adding that more funding is needed for future research.
Not so fast, warns Amanda D’Ambrosio:
Biological factors can likely predispose a baby to SIDS, which is further evidenced by this study. However, experts say these findings represent incremental progress, as opposed to a “breakthrough” set of findings that could change the game for SIDS prevention and detection.
Richard Goldstein, MD, a pediatric palliative care doctor at Boston Children’s who has conducted SIDS research, said that because so little research is done in this area, studies like this are important. However, sensationalizing those findings is not beneficial for the field.
Still, it’s very good news indeed that scientists are working hard and getting closer to Dr. Harrington’s vision of making SIDS “a thing of the past.” Let’s cheer them on.