January 10th, 2022
It was a “perfect storm” forecasted by practically every public health expert, pediatrician, and person who has seen this movie before: a sudden and severe spike of transmission and disease caused by a highly contagious and dangerous respiratory virus occurring a week or so after a family-oriented holiday full of traveling and gatherings. We saw surges of COVID-19 after the Christmas holiday last year, and after the July 4th holiday from the Delta variant, too. While Americans grew weary of following CDC (and let’s face it — common sense) recommendations as 2021 came to a close, it was inevitable what would happen to case rates that have now overwhelmed hospitals and physicians’ offices, drive-thru testing centers and pharmacies, ICUs and morgues.
The emergence and rapid dominance of Omicron, a variant that is even more contagious than Delta, is the biggest reason why children are getting sick with COVID-19 in higher numbers than before and filling up pediatric wards and children’s hospitals to capacity.
January is always a busy time for doctors’ offices, clinics, and hospitals. As expected every winter, influenza cases have been rising in recent weeks. In a year when too many stubbornly remain unvaccinated against COVID-19 and influenza, more are suffering from symptoms of “flurona”, a term used for describing patients infected with both viruses simultaneously, displacing last year’s favorite, “twindemic”, for that purpose.
Of course there are other viruses circulating in the community, and other conditions more common in winter than in other seasons — colds, RSV causing bronchiolitis in infants and toddlers, gastrointestinal illnesses and other assorted “kiddie crud”, asthma exacerbations, sled-riding and skiing accidents, weather-related hypothermia, frostbite, and vehicular trauma — that keep primary care doctors and emergency physicians busy all winter long. And pediatricians continue to struggle to get their patients back into the offices for regular checkups to assess growth and development and keep them up-to-date on lifesaving immunizations.
And no one should underestimate the impact the pandemic has had on the mental health of our patients, their caregivers, and medical providers and staff who care for them. Today, the need for mental health services to address the heightened levels of anxiety, depression, addiction, and suicide spiking most aggressively in young people has never been greater. Never have those services been more deficient, either.
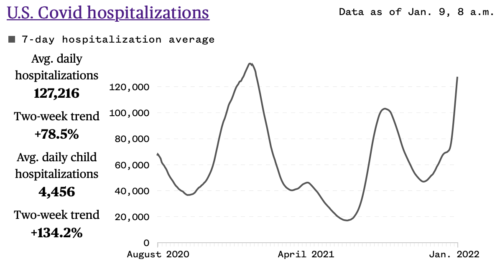
Daily pediatric hospital admissions of kids with COVID-19 are 134% higher than two weeks ago. Pediatric floors in community hospitals that have far more beds and resources reserved for adults than children, and children’s hospitals dedicated solely to pediatric health care are today filled to capacity. While Omicron appears to cause less severe illness in people who are infected, it needs to be said (again) that plenty of children and adults are still getting very sick and dying from it, a direct result of adults choosing to leave themselves and their children unprotected and vulnerable by rejecting exceedingly safe, effective, and widely available vaccines. Practically everyone who is hospitalized and dying from COVID-19 is unvaccinated — a sad fact that is entirely preventable.
As you can imagine (or perhaps you have already experienced it), pediatric offices everywhere have been slammed with phone calls seeking trusted assistance during this COVID spike. Parents are understandably on “high alert” for symptoms that might indicated a serious infection or complication from COVID-19 (or flu or RSV or something else) in their child. Many are calling for advice about COVID testing, especially if their child has been exposed to someone with COVID or if they develop symptoms consistent with COVID (the most common being congestion, a croupy cough, fever, headache, and fatigue). Parents may also be unclear about returning to school after observing quarantine or isolation protocols. Wearing a face mask IS necessary when coming out of quarantine and isolation; negative testing may not be. Only about 50% of kids between 12 and 18 and 16% between 5 and 11 are fully vaccinated against COVID-19, and many parents have decided they’ve waited long enough and now urgently wish to get their kids in for a shot.
Most parents we speak with understand how difficult these times are and react to long waits on hold with patience and empathy. They know our staff is overwhelmed but still doing the best they can to do what they do best: taking care of the needs of our patients and their families.
Remembering that the safety of patients, caregivers, providers, and staff is always our first priority, in order to protect everyone, it is vital that we know before a patient arrives at our office if they are potentially infectious with coronavirus.
Here are a few tips that can help parents decide when is the best time to call the pediatrician’s office during this busy winter season:
• Children with no symptoms and no exposure to a person with known or suspected COVID-19:
No need for testing or an office visit. For non-emergent concerns that don’t need immediate responses, please consider sending a message to the office through an electronic health record system like MyChart.
• Children with no symptoms but significant exposure:
If vaccinated in the last 6 months or boosted, no need to quarantine. Wear a face mask for 10 days and watch for symptoms. CDC currently recommends antigen testing 5 days after exposure.
If unvaccinated, not fully vaccinated, or vaccinated more than 6 months ago and no booster, quarantine for 5 days. Wear a mask and watch for symptoms. If no symptoms develop, end quarantine but wear a face mask for another 5 days. CDC currently recommends an antigen test 5 days after exposure in people who remain asymptomatic. Test immediately if symptoms of illness develop.
• Children with symptoms with or without significant exposure:
Please call the office and talk it over with a member of our office team. A provider will determine the need for an in-person or virtual office visit and/or testing. In most cases, a test will be recommended.
Symptomatic patients with a positive at-home test are considered positive. There is no need for further testing and no need to see a medical provider unless symptoms indicate the need for an evaluation (telehealth or in-person visit).
If any COVID test is positive, isolate for 5 days. If no symptoms or symptoms resolving (no fever) after 5 days, can end isolation, BUT continue to wear mask for 5 additional days. A negative antigen test is not required to end isolation after 5 days.
As always, call us if you need us. Follow us on Facebook and Instagram. Stay informed by reading credible, evidence-based sources. Listen to the experts. We’ll get through this together.