June 7th, 2022
It’s fair to say that the breaking news delivered on May 20 caught everyone off-guard:
An extremely rare disease called monkeypox, a much less severe cousin of smallpox, is spreading around the world. More than 250 cases have been reported in at least 16 countries, according to the World Health Organization. Experts say it is spread by close and prolonged contact with an infected individual.
At the time of the announcement there were more than 250 cases of monkeypox identified in at least 16 countries, including two cases in the United States. By the end of last week the outbreak had widened: 790 cases of the infection across 28 countries were identified, including 21 cases in 11 states here in the U.S. by CDC’s count
After nearly two-and-a-half years of being pummeled by the pandemic, it’s safe to say the reaction to a new outbreak of an infectious disease with a funny name has been predictable: “Monkeypox? What the…?”
The CDC provides us with some historical perspective:
Monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox.’ The first human case of monkeypox was recorded in 1970 in the Democratic Republic of Congo during a period of intensified effort to eliminate smallpox. Since then monkeypox has been reported in humans in other central and western African countries.
Emily Harris teaches “Monkeypox 101”:
Monkeypox is a zoonotic virus, meaning it is typically transmitted through close contact between an animal and human, often through a bite, scratch, or contact with the rash and with “fomites,” material like bedding or clothes contaminated with material from monkeypox lesions. Historically, human-to-human transmission has been less common. When person-to-person transmission does occur it is believed to be direct contact with lesion material or respiratory droplets.
Direct skin-to-skin contact is the primary mode of infectious transmission from one person to another. The virus can also be deposited from the skin lesions onto shared bedding, towels, and clothing and spread that way. Transmission by respiratory droplets (the primary route in which chickenpox is contagious, interestingly enough) is possible but less of a concern than direct skin contact.
David W. Kimberlin, M.D. says the rash looks similar to one caused by another virus familiar to veteran pediatricians: chickenpox.
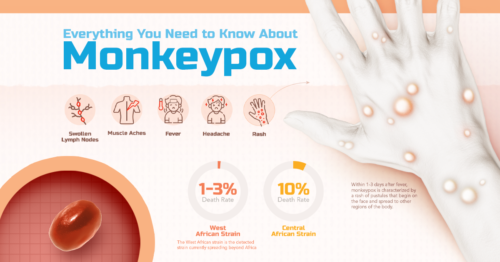
The telltale sign of monkeypox virus is how the rash looks and how the spots change over time. When the rash first appears, it looks like flat spots. All the spots change at the same time. They become raised bumps and then fluid-filled blisters that become pus-filled white/yellow sores. A person is contagious from the time symptoms develop until after scabs from the rash fall off. Before the rash appears, early signs may include:
• fever
• headache
• sore throat
• cough
• swollen lymph nodes
Dr. Kimberlin agrees with public health experts who say there is currently no cause for alarm about a virus which can kill up to 10% of its victims:
Cases mainly are reported in people who travel to central or west African countries and in people who have close or intimate contact with someone who is infected. Children under age 8 years, pregnant women and some people with immune conditions may be at higher risk of severe disease if they are in close direct contact with an infected person, or come in contact with clothes, bedding, etc., from someone with the rash of monkeypox.
Monkeypox sounds scary, but it is very, very unlikely that it will ever cause you any problems. It is much more difficult to transmit or acquire than COVID is. It is always good to be aware of health risks, but this is not one that should occupy much concern for you.
Read more about monkeypox from the American Academy of Pediatrics here, and follow the CDC’s surveillance of the disease here.