December 23rd, 2021
Even before the pandemic began, the average body mass index (BMI) for young adults 18-25 years of age was 27.7 — well within the range of overweight. We recently discovered that more children have joined the ranks of the overweight and obese during the pandemic.
Nearly half (46%) of American children between 5 and 11 years old were found to be either overweight or obese in 2020. Only a year before (prior to the start of the pandemic), 36% of kids 5-11 were considered overweight or obese. That’s a gain of ten percentage points in just one year!
Kristen Monaco points to new research showing that more than half of young American adults are now overweight or obese:
In 1976-1980, only 6.2% of young adults had obesity (BMI of 30 or higher). However, this number more than quintupled by 2017-2018, as nearly 33% of this age group had obesity, the analysis showed. The trend was likewise paired by a jump in overweight prevalence — increasing from 17.7% of this population during the first survey period to 23.6% by 2018.
All in all, this equated to 56.3% of all young adults having overweight or obesity during the most recent survey cycle.
When we looked last week at the BMI of all adults over 20, we found some pretty frightening numbers:
74% of American adults are either overweight or obese, according to the CDC. That means 3 out of 4 are likely to find themselves in serious trouble if they get infected with coronavirus, even before considering additional comorbidities. Maybe that helps explain 800,000 dead Americans in two years, just as the pandemic revs up in time for the holidays, with the Omicron variant aiming to overtake Delta as the dominant strain.
As the rates of overweight and obesity rise in children and adults, so do the risks for developing complications such as heart disease, cancer, and type 2 diabetes with its own long list of medical consequences.. Maureen Salamon says a large study recently revealed a very serious eye disease affecting alarming numbers of young adults with type 2 diabetes:
Almost half of young adults with type 2 diabetes develop a potentially blinding eye complication called diabetic retinopathy within a dozen years after diagnosis, new research reveals.
Diabetic retinopathy has long been a feared complication in children with juvenile or type 1 diabetes. But another study published earlier this month in JAMA Ophthalmology found that children with the more common type 2 diabetes actually have almost double the risk of developing diabetic retinopathy compared to those with type 1 diabetes. Salamon explains why this finding is so concerning:
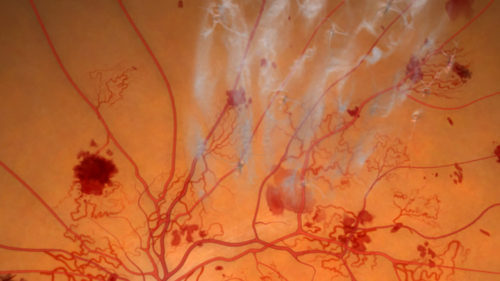
Diabetic retinopathy — the leading cause of blindness in working-age adults and one of the top reasons for preventable blindness — is characterized by damage to the blood vessels at the back of the eye. These abnormal vessels resemble scar tissue that can pull the retina out of place, causing blurriness, floaters, or severe vision loss.
In order to prevent diabetic retinopathy from damaging the eyes of young people, we need to prevent type 2 diabetes from developing. That can’t be done until we finally get a grip on the expanding obesity epidemic. One of the study’s authors tells Salamon where improvements can be made:
Even people without diabetes should be aware of this issue, she says.
“We need to work with families to overcome barriers to make sure healthy food is available to all, and that schools and kids can focus together on healthy eating and activity to help prevent these kids going on to have diabetes.”
And routine eye exams should also include the extra step of dilated retinal testing, Gubitosi-Klug says. With about 1 in 10 Americans diagnosed with diabetes, and another 88 million with prediabetes, such testing could reveal early signs of diabetic retinopathy or other dangerous vision changes.
(Proliferative Diabetic Retinopathy — Google Images)