December 28th, 2021
(Click image to enlarge)
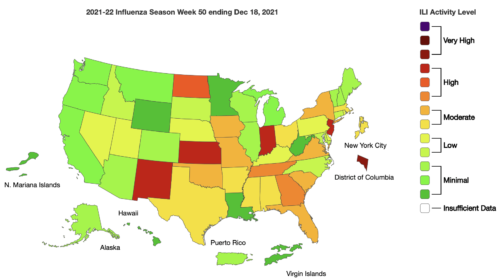
Seasonal influenza activity in the United States is increasing, including indicators that track hospitalizations. The amount of activity varies by region.
— CDC FluView (Key Updates for Week 50, ending December 18, 2021)
Just as the 2021-22 flu season is getting started, a new study published last week and awaiting peer-review suggests a “major mismatch” between the H3N2 influenza A strain currently circulating in the northern hemisphere and the H3N2 strain included in this year’s flu vaccine. This could leave people who receive a flu shot vulnerable to getting symptoms if they are exposed to the virus.
Every spring, scientists analyze the influenza viruses circulating in the southern hemisphere during their early winter season and make a prediction about which ones will make the trip North to pay us a visit during our cold and flu season. But every few years the virus undergoes an unexpected mutation, rendering the vaccine less effective in preventing illness.
Of course, the best case scenario after receiving any vaccine is never getting sick with the virus or bacteria the vaccine is designed to combat. But we know vaccines aren’t perfect in preventing illness, just like we know that everyone’s immune system isn’t perfect in producing enough protective antibodies after a shot to save us from potential misery. The good news, however, is even though we could get sick from the virus after vaccination, the researchers say it’s unlikely to cause a serious infection that leads to hospitalization, complications, and death. We’ve seen the same situation recently with COVID-19, where the current vaccines were well-matched against the Delta variant but not so much against the new mutation, Omicron. Even so, vaccines plus boosters are expected to reduce the chances of serious illness and death from both variants.
Cases of influenza and hospitalizations from the virus are on the increase in the U.S., according to the CDC’s Weekly Influenza Surveillance Report. The season’s first two pediatric deaths were reported last week, both from influenza A. The CDC adds:
• Influenza activity is increasing, with the eastern and central parts of the country seeing the largest increases and the western part of the country reporting lower levels of influenza virus circulation.
• The majority of influenza viruses detected are A(H3N2). Most influenza A(H3N2) infections have occurred among children and young adults ages 5-24 years; however, the proportion of infections occurring among adults age 25 years and older has been increasing.
The CDC sees early signs that the uptake of influenza vaccine is down this year compared to last, which was extraordinarily quiet due to pandemic restrictions on large public gatherings and face mask recommendations. All of the layers of protection that objectively reduce transmission of COVID-19 can also help prevent the spread of influenza and other seasonal respiratory viruses. And just like COVID-19, vaccination is still the best and most effective means to reduce illness and death from influenza, mutations and all:
The flu season is just getting started. There’s still time to get vaccinated. An annual flu vaccine is the best way to protect against flu and its potentially serious complications. CDC recommends everyone 6 months and older get a flu vaccine.
An antigenic mismatch between virus and vaccine makes it even more important to get a flu shot this year because we can expect more people to experience breakthrough cases of influenza than if there was a solid match.
It’s getting late, but not too late just yet. If you haven’t already, please help yourselves and each other by getting vaccinated today.
Read The PediaBlog’s preview of the 2021-22 influenza season here.